A troubling new analysis of health data spanning a decade reveals that Americans are increasingly struggling with memory, concentration, and decision-making—with young adults bearing the brunt of this dramatic shift.
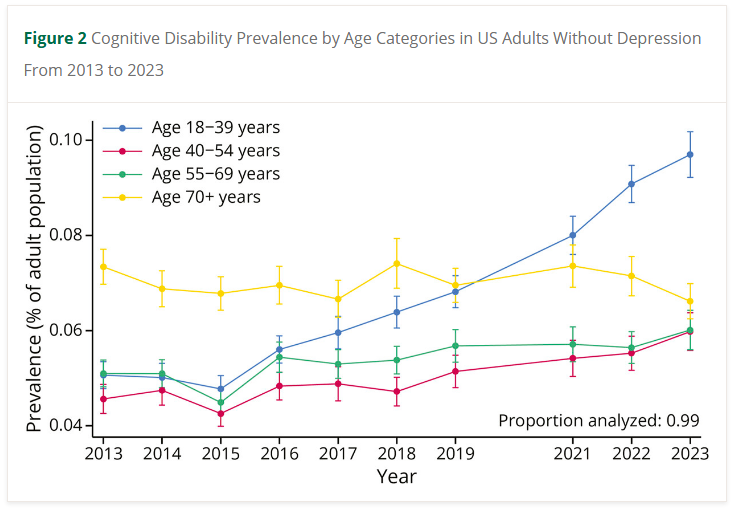
Researchers examining responses from more than 4.5 million U.S. adults found that self-reported cognitive difficulties nearly doubled among those aged 18-39 between 2013 and 2023. This age group saw rates climb from 5.1% to 9.7%, making younger adults the primary force behind rising cognitive disability nationwide.
The findings, published in the journal Neurology, paint a stark picture of generational change. While cognitive complaints among Americans age 70 and older actually declined slightly during the study period—from 7.3% to 6.6%—the surge among young people reversed what might otherwise have been a positive trend.
“The disproportionate growth in cognitive disability among younger adults seems to be the primary driver of the overall national trend,” the research team noted. “These findings warrant further investigation, given their potential long-term implications for population health, workforce productivity, and health care systems.”
The study drew on data from the Behavioral Risk Factor Surveillance System, an annual telephone survey that asks Americans whether they experience “serious difficulty concentrating, remembering, or making decisions because of a physical, mental, or emotional condition.” Researchers excluded people with diagnosed depression to better isolate non-psychiatric cognitive concerns.
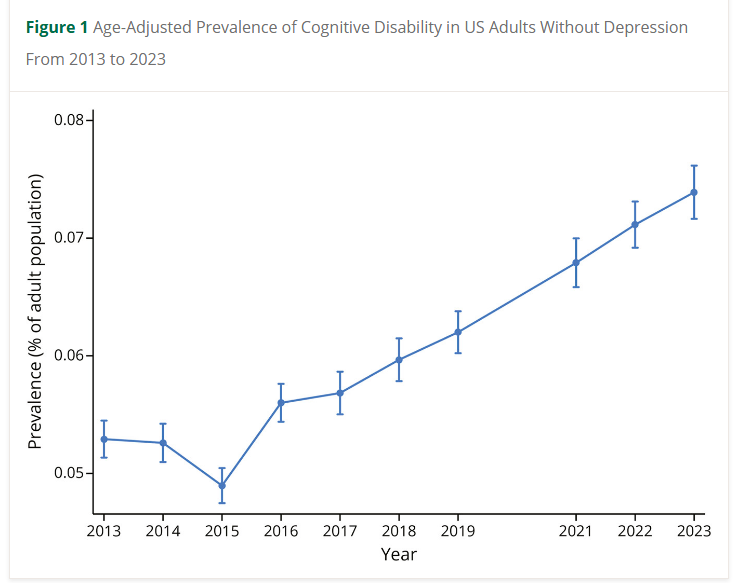
Overall, age-adjusted rates increased from 5.3% in 2013 to 7.4% in 2023, with statistically significant increases beginning in 2016 and continuing through the end of the study period.
The disparities extended far beyond age. American Indian and Alaska Native individuals reported the highest rates, jumping from 7.5% in 2013 to 11.2% by 2023. Black adults saw increases from 7.3% to 8.2%, while Hispanic adults experienced a rise from 6.8% to 9.9%. Asian Americans maintained the lowest rates, hovering between 3.9% and 4.8% throughout the decade.
Economic factors proved equally striking. Adults earning less than $35,000 annually reported rates climbing from 8.8% to 12.6%, while those making $75,000 or more saw a more modest increase from 1.8% to 3.9%. Education showed a similar pattern—those without high school diplomas reported rates jumping from 11.1% to 14.3%, compared to 2.1% to 3.6% among college graduates.
Geographic disparities emerged as well, with the South and Midwest reporting higher rates than the Northeast and West. U.S. territories showed particularly elevated numbers, reaching 9.1% by 2023.
When researchers examined how factors intersected, a surprising pattern emerged. Among younger White adults, rates more than doubled from 4.4% to 9.6%—the most dramatic increase of any demographic group studied. Younger Black and Hispanic adults also experienced significant rises, though not quite as steep.
The trend held across economic lines among young people. Even young adults with household incomes exceeding $75,000 saw rates triple from 2.2% to 6.6%. College-educated younger adults experienced nearly double the rate, rising from 3.7% to 7.3%. These patterns didn’t appear among older adults across any income or education level.
Gender differences proved minimal, though the direction shifted over time. Women reported slightly higher rates than men in 2013, but by 2023, men had edged ahead—a reversal that wasn’t statistically significant but suggested changing patterns worth monitoring.
Chronic health conditions correlated strongly with cognitive complaints throughout the study. Adults with a history of stroke reported the highest rates at 18.2% in 2023. Those with hypertension, diabetes, and high cholesterol also showed elevated numbers compared to people without these conditions.
The researchers emphasized that self-reported cognitive difficulty differs fundamentally from diagnosed conditions like dementia or mild cognitive impairment. Rather than capturing clinical disease, these responses reflect people’s lived experience of functional challenges in their daily lives.
“Self-reported cognitive disability reflects individuals’ perceptions of difficulty concentrating, remembering, or making decisions,” the authors explained. “Although self-reported cognitive disability is not a clinically validated diagnosis, its rising prevalence carries important implications for public health.”
Several factors may help explain why younger adults increasingly report these struggles. Growing awareness and reduced stigma around cognitive and mental health issues may make people more willing to acknowledge difficulties. Economic uncertainty, job market pressures, and workplace changes—including heavy reliance on digital technology—could contribute to cognitive strain.
The relatively stable or declining rates among older adults might reflect decades of progress managing cardiovascular risk factors known to affect brain health. Better education and healthcare access among older generations could also play a role.
However, the survey design excludes a crucial population: people in nursing homes or with severe impairments who can’t complete a 20-minute phone interview. As dementia rates rise nationally, a growing number of older adults with the most serious cognitive problems simply aren’t captured in these numbers.
The researchers called for comprehensive public health strategies addressing root causes of these disparities. Improving educational opportunities, expanding access to affordable healthcare, and tackling structural barriers faced by disadvantaged communities emerged as essential priorities.
The study excluded 2020 data due to pandemic-related survey disruptions, leaving questions about COVID-19’s immediate cognitive impact. But the clear upward trend beginning in 2016—well before the pandemic—suggests deeper forces at work.
“Addressing social determinants of health and improving access to care for vulnerable populations will be essential to mitigate the rising burden of cognitive disability and its associated challenges,” the researchers concluded.
For younger Americans especially, the message appears clear: a growing number feel their minds aren’t working as they should. Whether that reflects changing perceptions, new environmental pressures, or actual declines in cognitive function remains an urgent question demanding answers.
References
1. Ka-Ho Wong, Christopher D. Anderson, and Cecilia T. Chung, ‘Rising Cognitive Disability as a Public Health Concern Among US Adults: Trends From the Behavioral Risk Factor Surveillance System, 2013–2023’, Neurology (2025).
2. Centers for Disease Control and Prevention (CDC), Behavioral Risk Factor Surveillance System Survey Data and Documentation (Atlanta: U.S. Department of Health and Human Services, 2013–2023), available at: https://www.cdc.gov/brfss/
[accessed 10 November 2025].
3. U.S. Census Bureau, American Community Survey: Demographic and Economic Data, 2013–2023 (Washington, D.C.: U.S. Department of Commerce, 2024).
4. National Center for Health Statistics (NCHS), Health, United States, 2023: Annual Report on Trends in Health Statistics (Hyattsville, MD: U.S. Department of Health and Human Services, 2024).
5. Alzheimer’s Association, 2024 Alzheimer’s Disease Facts and Figures (Chicago, IL: Alzheimer’s Association, 2024).
6. Laura B. Zahodne and Jennifer J. Manly, ‘Social Determinants and Cognitive Aging: A Life-Course Perspective’, Annual Review of Gerontology and Geriatrics, vol. 42 (2023), pp. 55–78.
7. U.S. Department of Labor, Economic Stress and Workforce Mental Health Report (Washington, D.C.: Bureau of Labor Statistics, 2024).
8. Vivek H. Murthy, ‘Our Epidemic of Loneliness and Isolation: The U.S. Surgeon General’s Advisory’ (Washington, D.C.: U.S. Department of Health and Human Services, 2023).
9. Rajita Sinha, ‘Chronic Stress, Cognitive Function, and Brain Health in the Modern Age’, Nature Reviews Neuroscience, vol. 25, no. 2 (2024), pp. 89–102.
10. World Health Organization (WHO), Social Determinants of Mental Health (Geneva: WHO Press, 2023).